Well, we are between months four and five post ATG at this
point, but I held off on posting because I was hoping to have more information
to share.
We have seen a very slight improvement in Ryan’s platelet
count. And by “improvement”, I mean that
we have been able to space out the time between transfusions just a little
bit. He was requiring platelet transfusions
each week, up until Halloween day, when we went to his clinic appointment expecting
him to need a transfusion, but his platelet count was 32,000. As a reminder, a normal platelet count for a
child Ryan’s age should be 250,000-550,000.
Even though 32,000 is well below a normal range, doctors do not like to
transfuse until a patient is around 10,000 in order to limit the number of
transfusions they receive, which can increase antibodies in their system and,
among other things, increase the risk of bone marrow transplant rejection and
graft verses host disease (GVHD) if the patient later has a transplant. Anything under 10,000 is considered in the
“danger zone” where there is a high risk of hemorrhage.
So, we skipped a transfusion on Halloween and the doctor
decided we could wait another week.
Within a few days, I started noticing petechiae (red dots that indicate
low platelets) under Ryan’s Eyes and bruises on his arms and legs. By the end of the 2-week period his platelet
count was down to 6,000.
A week later, we finally were able to have our appointment
with the doctors from Fred Hutchinson Cancer
Research Center
in Seattle . The two doctors we met with specialize in,
and research, bone marrow failure diseases.
I was a little bit disappointed because my expectation of the
appointment was that the doctors had already received all of the tests Ryan
previously had and that they would be making a recommendation regarding whether
we should pursue a bone marrow transplant.
Instead, we were basically starting over with new doctors - answering
questions, giving family history, etc.
They told us they wanted to do several more genetic tests
and a new bone marrow biopsy. They also
asked our permission to map Ryan’s genome, which I think is really cool and I
am curious to know if any new information comes out of that (although we were
told that sometimes they get information that they don’t know what to do with). One of the reasons for all of the genetic
testing is that, if they do find something genetic, and Ryan does proceed to
transplant, it could help the transplant team determine the pre-conditioning
regimen. Certain chemotherapy drugs can
be more toxic if you have certain genetic conditions.
The doctors were great to speak with; it just wasn't what I
expected the appointment to be all about. The lesson learned for me is to ask
more questions in advance about what to expect. I had created an entire page
full of questions about the transplant process, but that just isn't at all why
we were there. At the end of the 5-hour appointment, they took about 10
vials of blood for various tests and scheduled a bone marrow biopsy for
November 21st (tomorrow at this point). Ryan’s platelet count that day was 25,000 so
we were able to skip another platelet transfusion.
I tend to report a lot on Ryan’s platelet count, and that is
because platelets are basically the first thing to go. They only have a lifespan of about 6 days,
where red blood cells can last about 35 days.
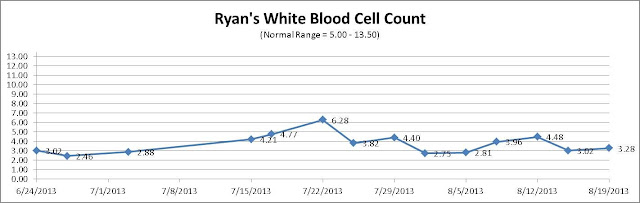
That is why platelet counts can go up and down so quickly. I should mention though, that there has also
not been much improvement in Ryan's white and red cell counts. Ryan is still requiring red cell transfusions
about every 3 weeks. White cells cannot
be transfused and his remain below normal.
One of the other numbers I pay attention to is his neutrophil count. Neutrophils are a type of white blood cell
that fights off infection. The normal
range for Ryan should be 1,500-8,500. He
had a few weeks where his went over 1,000 but they keep dipping back down. He has been running in the 700-800 range
lately.
Ryan ended up not getting platelets last week like we thought he would, however, by the
weekend, it started to show. He had
invitations to birthday parties on both Saturday and Sunday, and I decided not
to tell him about either one. I knew he
would want to go, but I was worried that he would get hurt or pick up germs at
the events, which could easily lead to a trip to the ER. One party was at Chuck E Cheese and the other
was at a Little Gym. I felt bad that he
had to miss out, but I decided not to risk it.
Then, Saturday, he accidentally whacked himself with a
lightweight bamboo back scratcher and it gave him a black eye. This was followed by two other minor bumps
while playing that resulted in bruises on his forehead. The level of impact from these “accidents” to
a person with a normal platelet count probably would have either left a slight
red mark for a few minutes, or no mark at all.
But, when they happen to a Ryan, with low platelets, they result in him
looking a little beat up. Here is a
picture of his eye:
What’s next?
Tomorrow Ryan will have a new bone marrow biopsy. The only other bone marrow biopsy he had was
when he was admitted to the hospital at the time of diagnosis (June 24,
2013). They will be looking for any signs of improvement and also any signs of other concerning items in his remaining cells such as PNH clones, MDS, or Leukemia.
One of the main things they
look at in a biopsy is “bone marrow cellularity”. Cellularity is basically the percentage
of bone marrow that contains healthy cells as opposed to adipose tissue. At birth, cellularity is approximately 100
percent and then declines with time as people age. Cellularity in a healthy adult is
approximately 50%. Cellularity in a
healthy 4-year old should be around 70%-80%.
Ryan’s cellularity in June was less than 5%. Here is what the bone marrow of a person with
Aplastic Anemia looks like in comparison to healthy bone marrow:
Bone Marrow of an Aplastic Anemia Patient:
Healthy Bone Marrow:
After the biopsy, we will continue our regular weekly clinic
visits and then have a consultation on December 9th with the Seattle
Cancer Care Alliance Transplant Team.
This is the appointment where we will hear about Ryan’s test results,
options for bone marrow transplant, discuss all of the risks, worst case
scenarios, etc. We will get the results
of the “World Book” search (international bone marrow donor search) and find out if Ryan has a potential donor. We will also meet with a financial counselor
(because, as you can imagine, it is expensive and there is quite a bit out of
pocket that is not covered by insurance) and, last, we will tour the facility.
Please continue to keep us in your thoughts and
prayers. Although this journey has
already felt very long, I fear that it is only really just beginning.